Learn about and advocate against these harmful programs for people with commercial insurance.
In recent years, commercial health insurers have adopted programs and policies that are hurting patients. These programs limit access to medications, increasing the amount patients have to pay out-of-pocket for their care.
Unfortunately, patients often don’t know that these programs are part of their health plans. They often learn about the programs when their insurance company denies medications. Or they are at the pharmacy counter and are surprised by their out-of-pocket cost.
We invite you to learn about three of these harmful programs below, including copay accumulators, copay maximizers, and alternative funding programs. These programs may prevent patients from adhering to treatment. So, it is important that patients and healthcare professionals understand how they work. In addition, learning how they can advocate against these harmful programs.
Copay accumulators
What is a copay accumulator?
Copay accumulators are programs used by insurance plans that affect how copay assistance is applied to deductibles and out-of-pocket costs.
People living with serious illnesses are often prescribed medications with high out-of-pocket costs. Many patients find it challenging to afford these costs. This is why they often turn to financial assistance provided by pharmaceutical manufacturer programs, charitable foundations, friends and family, and faith-based communities. This financial help usually counts toward the patient’s annual deductible or out-of-pocket maximum, based on their health plan.
But that isn’t the case for patients whose health plans have a copay accumulator program in place.
How copay accumulators work
Copay accumulator programs are typically offered by the plan’s pharmacy benefit manager. These programs allow patients to use financial assistance to pay for the medication. However any third-party contributions, like the value of a manufacturer coupon, don’t count toward the patient’s deductible or annual out-of-pocket maximum. Once a patient has exhausted their copay assistance funds, they are still responsible for their entire deductible (minus the cost-sharing amount set by manufacturers for patients using the card) and cost-sharing up to their original out-of-pocket maximum. These programs are complex, so we’ve shared two scenarios below to help explain how they work.
For example, let’s consider a patient named Arthur, who is living with a chronic illness. Arthur has an annual deductible of $2,500 and a $500 manufacturer copay coupon for his medication.
- If Arthur’s plan does not have a copay accumulator program, the $500 coupon will count toward his annual deductible: $2,500 – $500 = $2,000. Arthur will be responsible for the remaining $2,000 before reaching his annual limit.
- If Arthur’s plan has a copay accumulator program, the $500 coupon will not count toward his annual deductible: $2,500 – 0 = $2,500. Arthur must pay the full $2,500 before satisfying his annual deductible.
When health plans include copay accumulator programs, patients pay more out of pocket for their treatment. It also takes them longer to reach their annual deductible and out-of-pocket limits.
The Crohn’s & Colitis Foundation shared a similar example of how copay accumulators work in the illustration below:

The impact of copay accumulators on patients
Unfortunately, copay accumulator programs are often put in place with little or no notice or education for patients. Accumulator programs negatively impact patients in several ways:
- They can lead to poorer health outcomes and may add costs to the entire health system. This happens when patients choose to not start taking a medication at all, or to skip doses and not follow the treatment as prescribed by their healthcare provider.
- They result in increased costs for the patient. This can be particularly challenging for people with high-deductible health plans.
Copay Maximizers
What are copay maximizer programs?
Copay maximizer programs allow health insurance plans to “maximize” the value from copay assistance programs. They do this by adjusting a patient’s cost-sharing to a maximum amount. These programs require patients to enroll with a third-party administrator before they can fill prescriptions. The administrator determines the maximum amount of manufacturer copay assistance available and advises the plan to set monthly copays accordingly. The copay can be divided evenly throughout the year, or the plan may set higher copays at the beginning of the year.
With maximizer programs, copay support provided by the manufacturer does not apply towards the patient’s deductible or out-of-pocket maximum. Once assistance has been exhausted, the maximizer program adjusts the patient’s copay to an amount determined by the pharmacy benefit manager. This is often set at the same amount the patient was paying with manufacturer assistance.
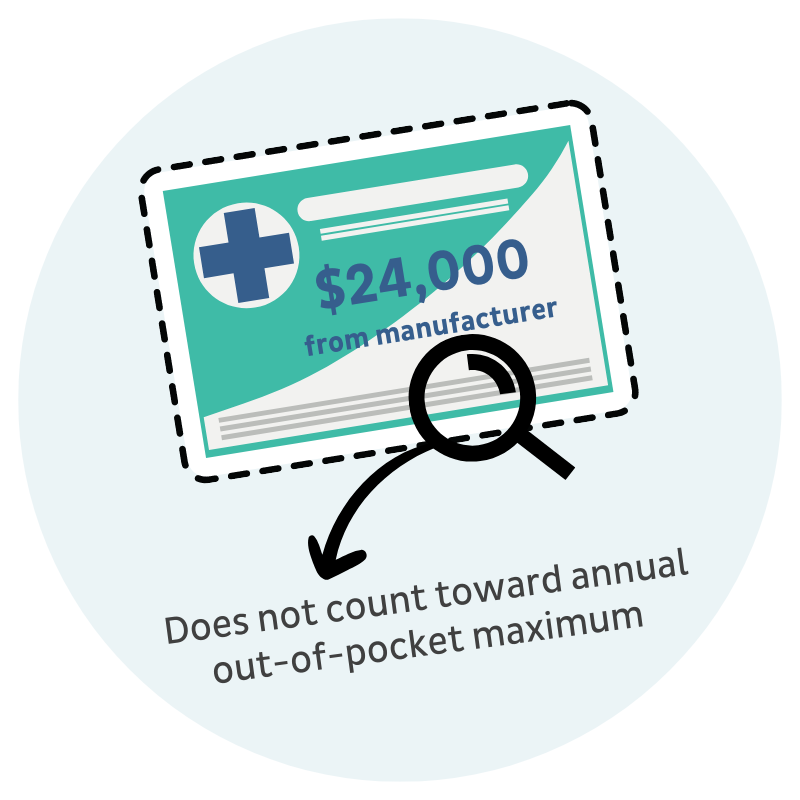
For example, let’s say that Ariel needs a specialty medication for her rare disease. There is $24,000 in manufacturer copay assistance available per year for her medication. Ariel’s health plan determines that her copay is at least $2,000 per month—$24,000 in available copay assistance divided by 12 months in the plan year.
Plans then notify patients, like Ariel, that they can avoid high cost-sharing by signing up for a copay maximizer program. The program applies manufacturer’s assistance to the patient’s prescription costs.
However, if a patient does not join the program and uses the manufacturer’s assistance, they will be responsible for all the cost-sharing.
Whether or not they use a copay maximizer program or self-pay, none of the payments will count toward their annual out-of-pocket maximum.
In Ariel’s example from above, she has two choices:
- She can join the copay maximizer program and use a manufacturer’s coupon to cover the $2,000+ monthly copay. She will have little or no upfront cost for her medication, but these payments will not apply to her annual out-of-pocket maximum.
- Or she can choose not to join the copay maximizer program and face the $2,000+ copay each month on her own. Her payments will not apply to her annual out-of-pocket maximum in this scenario either.
The impact of copay maximizers on patients
Maximizer programs negatively impact patients in several ways:
- They disproportionately impact individuals who are seriously or chronically ill. Faced with increased out-of-pocket costs, patients may choose not to start taking a medication at all, or to skip doses and not follow the treatment as prescribed by their doctor. This may lead to poorer health outcomes.
- They may cause patients to face significant out-of-pocket costs if they don’t sign up for a maximizer program. These costs may exceed their plan’s out of pocket maximums. Their costs may also exceed the out-of-pocket maximums established by the Affordable Care Act.
- They hurt patients in the long run. This is due to payments coming from the manufacturer copay assistance program not applying to a patient’s annual deductible.
- They are also why some health plans are restricting access to essential health benefits. Plans are claiming that more and more specialty medications are non-essential and therefore do not have coverage. Non-essential health benefit schemes like copay maximizers violate the Affordable Care Act (ACA). Under the ACA, patient contributions for essential health benefits, like prescription drugs, must count towards their annual out-of-pocket limits. (Read more about essential health benefits below)
What are essential health benefits under the ACA?
Prescription drugs are one of the ten essential health benefit (EHB) categories listed in the Affordable Care Act (ACA). The ACA does not specifically define “prescription drugs.” However, it refers to them broadly as FDA-approved drugs. Specialty medications are FDA-approved drugs, often prescribed to treat life-threatening, chronic, and rare diseases.
Health plans can adopt their own definition of EHBs. But their definition must be consistent with guidelines from the U.S. Department of Health and Human Services (HHS). To date, HHS has stated that plans can only exclude a name-brand prescription drug from coverage when the plan offers a generic alternative.
So that means when a health plan broadly categorizes specialty medications as non-essential health benefits without a generic alternative available, they are using an unauthorized definition of prescription drugs.
Violation of ACA’s cost-sharing requirements
Under the Affordable Care Act (ACA), all essential health benefits, including prescription drugs, have annual limits on cost-sharing, unless an exception exists. Cost-sharing includes deductibles, coinsurance, copayments, and similar charges.
The HHS has also stated that if a patient pays for and receives a prescription medication that isn’t covered under the general health plan, the plan must consider this medication an essential health benefit and count the patient’s out-of-pocket payments toward the plan’s annual limit on cost-sharing. So, programs that prevent payments for specialty medications from counting towards a patient’s annual limits are not in compliance with the ACA’s cost-sharing requirements.
What’s being done to protect people from copay accumulators and copay maximizer programs?
State legislation
To date, 25 states, the District of Columbia, and Puerto Rico have passed legislation to ban these programs.
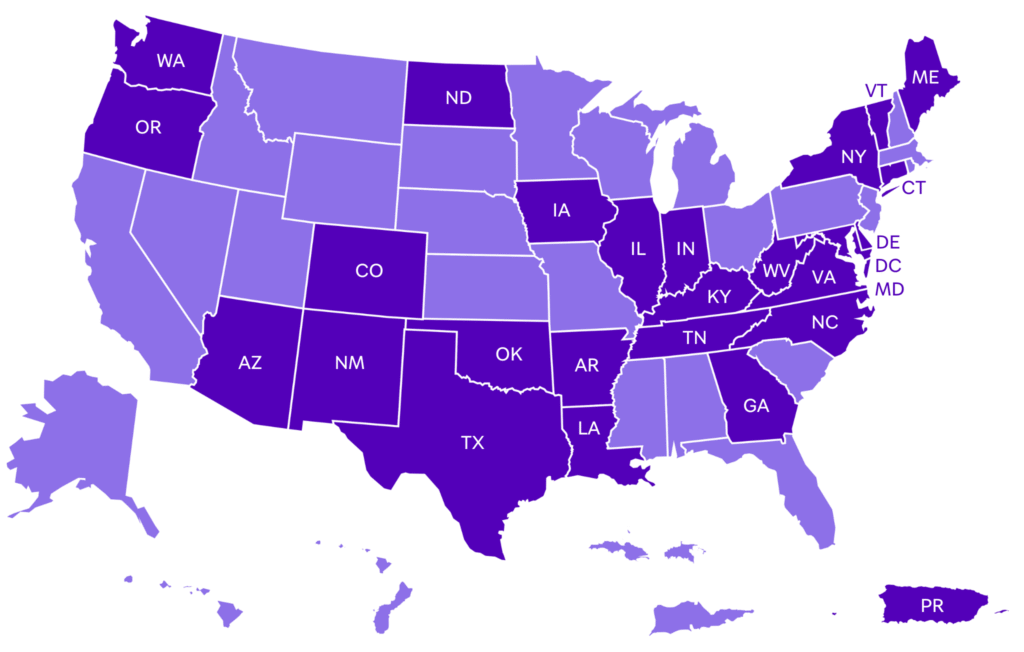
In each of these states and territories, legislation requires insurers to count copay assistance paid by or on behalf of a patient towards their annual deductible and out-of-pocket maximum. The laws primarily target copay accumulators but some also ban copay maximizers.
State legislation applies to state-regulated individual and family plans and fully funded small group health plans. It does not apply to self-funded employer plans or large group plans. Unfortunately, state legislation does not stop plans from determining that specialty medications are non-essential health benefits.
Federal regulations
Every year, the U.S. Department of Health and Human Services (HHS) publishes the Notice of Benefit and Payment Parameters (NBPP) for the following year. NBPP rules generally apply to individual and small-group market plans, particularly those offered through the ACA marketplaces. They do not apply to large group plans or self-insured employer plans.
The 2020 NBPP rule required insurers to count copay assistance towards patients’ deductibles and out-of-pocket maximums, unless assistance was provided for brand-name drugs with an available generic equivalent. The 2021 NBPP reversed this requirement, permitting health plans to exclude copay assistance from counting toward cost-sharing limits, regardless of generic availability.
In 2023, the US District Court for the District of Columbia struck down the 2021 NBPP rule, reinstating 2020 standards. HHS has declined to enforce these standards prior to future rulemaking.
The 2025 NBPP rule clarified that all covered prescription drugs are considered Essential Health Benefits, requiring plans to adhere to the ACA’s cost-sharing limits.
For the 2026 NBPP rule, CMS announced an intention of rulemaking with HHS and the Departments of Labor and Treasury and signaled their intent to extend similar standards to large-group and employer-sponsored plans.
Moving forward, it is our hope that rulemaking will align with 2020 NBPP policy, requiring plans to count patient assistance programs toward deductibles unless a generic equivalent is available. Rulemaking should also address the EHB loophole in the large-group and self-insured group plans and classify all covered medicines as EHBs in these plans.
Federal legislation can ban copay accumulator and maximizer programs
While state legislation applies to state-regulated individual and family plans and fully funded small group health plans, it does not apply to self-funded employer plans or large group plans. Unfortunately, state legislation does not stop plans from determining that items and services, like specialty medications, are non-essential health benefits.
At the federal level, the Help Ensure Lower Patient (HELP) Copays Act will be most impactful.
The HELP Copays Act requires health plans to count the value of copay assistance toward a patient’s cost-sharing requirements. The bill clarifies the Affordable Care Act definition of cost-sharing to ensure payments made “by or on behalf of” patients count towards their annual deductible and/or out-of-pocket maximum.
The legislation also states that any item or service covered under a plan is an essential health benefit and that cost-sharing for these items must count towards a patient’s out-of-pocket maximum.
The HELP Copays Act was re-introduced (S.864) by Senators Tim Kaine (D-VA) and Roger Marshall (R-KS) in March 2025.
Three things you can do about copay accumulator and maximizer programs
#1 – Understand your policy
You should become familiar with your insurance policy documents and know if your plan includes a copay accumulator or maximizer program. People with employer-sponsored insurance plans, particularly people enrolled in high-deductible health plans (HDHPs), are most likely to have a copay accumulator or maximizer plan in their policy. HDHPs have become popular as employers and insurers try to lower their costs. When selecting insurance plans, it is important to understand your health plan’s deductible and your cost-sharing requirements.
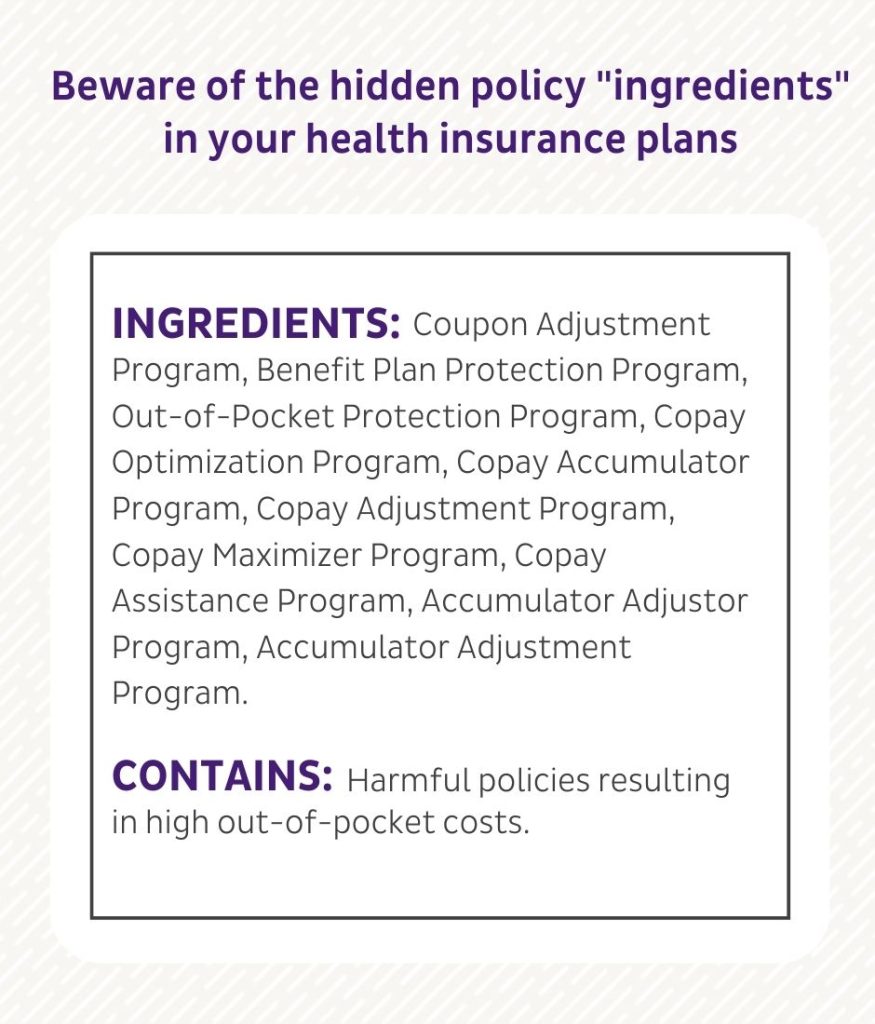
Unfortunately, it can be quite difficult for patients to know if their plan has a copay accumulator or maximizer program in place—language differs from plan to plan.
These terms can all mean a plan includes a copay accumulator or maximizer policy:
- Copay accumulator (adjustment) program
- Copay maximizer program
- Benefit plan protection program
- Out-of-pocket protection program
- True accumulation
- Variable copayment
- Out-of-pocket maximum calculation
- Primary coupon adjustment
#2 – Become an advocate
Ask your elected officials to support The HELP Copays Act and ban copay accumulator programs.
If you live in a state that has not banned copay accumulators:
- Contact your House representative
- Contact your state’s insurance department
- Tell your employer! It is possible that your employer may not be aware that they signed up for this program and may not realize the potential negative impact of the program has on their employees.
#3 – Share your story with PAN
If you have experienced the impact of a copay accumulator or maximizer program, we would love to hear from you. Your story helps others understand the impact of these programs.
Alternative funding programs
Understanding alternative funding and specialty drug carve out programs
Health plan sponsors, like employers that fund their own health coverage, may use alternative funding programs to save money by excluding some or all specialty medications from coverage, labeling them as non-essential health benefits. Since the health plan does not cover these specialty medications, a patient’s out-of-pocket spending will not count toward their annual deductible. Patients are then directed to alternative funding programs—also known as specialty drug carve out programs— operated by vendors that are separate from their health plan and are not health insurance.
These vendors work to connect patients with financial assistance through a drug manufacturer or charitable assistance program, disguising patients as uninsured, if necessary. Technically, these patients have no coverage for these medications. Vendors may even direct patients to illegally import medications internationally. But help paying for these medications is not guaranteed from any of these sources.
How these programs work:
- The patient is told that they must enroll in an alternative funding program and is referred to a private company, often called an alternative funding vendor. Vendors operate separately from the patient’s health plan.
- The vendor contacts the patient and offers to help find an assistance program to access their specialty medications.
- If the patient agrees to work with the vendor, the patient may be able to get their medication for little or no out-of-pocket costs if a patient assistance program is available and if the patient qualifies.
- The vendor collects the patient’s personal information, such as household size and annual income, to determine the type of third-party financial assistance the patient is eligible for.
- Vendors then determine whether patients are eligible for manufacturer copay assistance programs, charitable assistance programs, or international importation programs.
- The vendor helps patients disguise themselves as uninsured so they can apply for patient assistance programs to cover the cost of the prescriptions. (Keep in mind that while these patients have health coverage, their plan states that they are not covered for the specialty medications they need.)
- If no patient assistance program is available or if the patient fails to qualify, then the patient can be denied access to the medication or forced to pay out of pocket on their own. If assistance can’t be found or a patient can’t qualify, their health plan also has the option to override the original designation as a non-essential benefit, which allows the patient to resubmit a request for prior authorization for their specialty medications.
- If the patient refuses to work with the alternative funding vendor, then the patient will be denied access to the medication unless they self-pay.
- If the patient does not enroll, they will be responsible for 100 percent of the cost of the medication that is deemed non-essential. As a non-essential medication, any cost paid for the medication by or on behalf of the patient will not count towards their deductible or annual limit on cost-sharing.
- If the patient is eligible for a different program, like one that imports internationally, then the patient will receive their medication through that source. Some vendors will try to get products from pharmacies located outside the United States, but this is not permitted based on guidance from the Food and Drug Administration (FDA).
Access to specialty medications prescribed by health care professionals should be deemed an essential health benefit, and their costs should be covered by health plans. Patient assistance programs should be reserved for those who meet their specific eligibility criteria, based on need.
Federal legislation can ban alternative funding programs
Currently, there is no legislation pending that would prohibit the use of alternative funding programs. It is possible that there will be growing interest from Congress and the patient advocacy community stands ready to advocate to ban these harmful programs.
Three things you can do about alternative funding programs:
#1 – Understand your policy
If your plan has told you that your specialty medication is not essential, or that specialty drugs are excluded from the plan’s formulary and that another company can help you find financial assistance, then you may be involved in an alternative funding program scheme. When selecting insurance plans, it is important that you understand the health plan’s policy on including/excluding specialty medications on formulary.
#2 – Become an advocate
Let your elected officials know that alternative funding programs harm patients and should be abolished. Reach out to your members of Congress to share your story.
#3 – Share your story with PAN
As alternative funding programs become more common, one of the most important things we can do is track and share stories about how these programs are negatively impacting patient care. With alternative funding programs, patients face delays in their care and have the additional burden of sharing personal, financial, and medical information with external private companies just so that they try to find funding. If funding sources are not found, patients may have to delay starting their treatment, which could impact their health outcomes. If you have experienced an alternative funding program, we invite you to share your story.
-
Subscribe to news
Sign up to receive PAN news, from helpful articles to action alerts.
Subscribe today -
-